Many people experience or know someone who suffers from migraine headaches. Abdominal migraine — or stomach migraine — is rarer and less understood. It mainly affects children, causing stomach pain, nausea and vomiting. Around 1-4% of all children have abdominal migraine.
While this migraine type’s causes are uncertain and it can be challenging to diagnose, effective treatments are available. If you believe you or your child has abdominal migraine, this guide will help you understand the condition and plan your next steps.
What are abdominal migraines vs. migraine headaches?
It’s possible to experience abdominal migraine and a migraine headache at the same time, but they are distinct conditions. Abdominal migraine mainly presents with stomach symptoms and without a headache. This distinguishes it from a regular migraine attack, which has a throbbing headache as its most prominent symptom.
Abdominal migraine also tends to impact a younger population, being most common in children under 10 with an average onset age of 7. Migraine headache is most prevalent in adults aged 20-50. At the same time, there are similarities between these conditions:
- Both are more common in females than males.
- Migraine headaches often present with nausea or vomiting.
- Abdominal headaches sometimes present with a headache.
- Though abdominal migraine can subside after only one hour, both can last up to 72 hours.
- Many of the same triggers set off both conditions, and many of the same treatments relieve both.
These and other factors suggest a link between abdominal migraine and migraine headaches. Researchers still have questions about how this link works, though.
Abdominal migraine causes
Researchers are uncertain about what causes abdominal migraine. The leading idea is that an oversensitive nervous system sends unusual chemical signals in response to triggers. These signals — neurotransmitters — then contribute to abdominal pain. The main neurotransmitters that could be culprits are histamine and serotonin.
Right now, this is only a hypothesis. The cause of abdominal migraine is uncertain, but research has identified several risk factors and triggers that can help you better understand root causes.
Risk factors
Certain people are more likely to experience abdominal migraine than others. Prominent statistical risk factors include the following:
- Family history: Children with a family history of migraine headaches are more likely to have abdominal migraine. Over 65% of children with abdominal migraine have a parent or sibling with migraine headaches.
- Age: Abdominal migraine is more common in children aged 3-10 than adults. Most children with abdominal migraine grow out of it within a couple of years, but up to 70% later develop migraine headaches.
- Sex: Females are more likely to have abdominal migraine than males.
- Mental health: Anxiety and depression can increase one’s risk of developing abdominal migraine.
Common triggers
Several environmental or lifestyle triggers can set off abdominal migraine attacks. Using a migraine diary to find patterns in these triggers can help avoid them. The most common abdominal migraine triggers include the following:
- Stress
- Insufficient or irregular sleep
- Missing meals
- Dehydration
- Motion sickness
- Overexertion
- High-amine foods like chocolate, cheese and processed meats
- Foods with MSG or other artificial flavoring or coloring
- Harsh or flashing light
- Consuming over 200 milligrams of caffeine (2 or more cups of instant coffee)
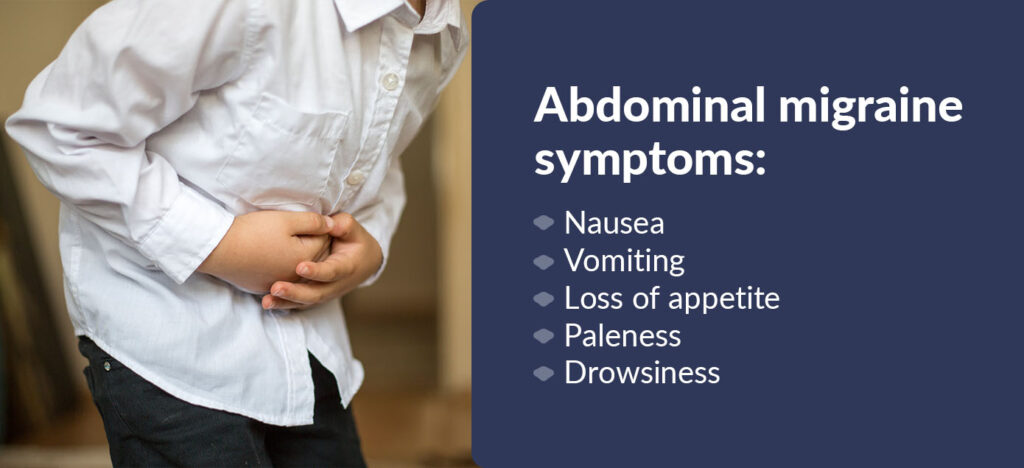
Abdominal migraine symptoms
Abdominal migraine involves recurring attacks of moderate to severe dull stomach ache, continuing for 1 to 72 hours. The pain is normally concentrated in the middle of the belly, around the navel.
Other symptoms sometimes accompany the pain of migraine in the stomach, including:
- Nausea.
- Vomiting.
- Loss of appetite.
- Paleness.
- Drowsiness.
Rarer symptoms include:
- Headaches.
- Light sensitivity.
- Sound sensitivity.
Weeks or months can go by between migraine episodes. People with abdominal migraine typically experience no symptoms between episodes. This distinguishes abdominal migraine from other gastrointestinal conditions with more constant symptoms.
If abdominal pain causes difficulty eating or moving for an extended time, seek emergency care promptly.
Diagnosing abdominal migraine
No single test can confirm whether a patient has abdominal migraine. Doctors consider the type, severity and frequency of a patient’s symptoms. If you have a migraine journal that records your or your child’s symptoms, this information will help your doctor. They’ll also use an examination and tests to rule out other conditions with overlapping symptoms, such as:
- Cyclic vomiting syndrome.
- Stomach ulcers.
- Crohn’s disease.
- Irritable bowel syndrome.
- Bladder or kidney conditions.
Treatment options for abdominal migraine
If a doctor diagnoses you or your child with abdominal migraine, you have several treatment options for prevention and relief. Preventive solutions to decrease abdominal migraine frequency include:
- Stress management: Cognitive behavioral therapy (CBT) can help develop healthy stress-management tools. Effective stress management can reduce migraine days.
- Sleep hygiene: Avoid screens around bedtime and maintain a consistent sleep schedule. Elementary school-aged kids need 9 to 12 hours of sleep per day, while adults need 7 to 9.
- Strategic nutrition: Identify and avoid common trigger foods. Use a migraine journal to track foods that seem to trigger abdominal migraine in you or your child.
- Sensitive traveling: Reduce migraine-triggering motion sickness by making regular stops on long drives.
- Pizotifen: A benzocycloheptene-based drug.
- Cyproheptadine: An anti-histamine.
- Flunarazine: A calcium channel blocker.
- Propranolol: A beta-blocker is also used to lower blood pressure.
Your doctor may also recommend an acute treatment to relieve abdominal migraine symptoms. Explore the options available:
- Pain relievers: These include ibuprofen, aspirin or acetaminophen.
- Triptans: Medicines in this family can help stop symptoms from progressing.
- Anti-nausea drugs: These can relieve the discomfort of nausea and prevent vomiting.
- Removing triggers: Address anything that could be triggering or aggravating the episode. For example, if you’ve missed a meal, try eating something nutritious. If possible, move to a quiet, dark space and try to sleep.
Before starting any new medication, ensure you have a doctor’s approval and understand the potential side effects.
Get more answers about migraine with CEFALY
If you or your child has abdominal migraine, straightforward information can help you manage it and enhance your quality of life. Your best resource for your family’s health is your primary care provider. But you can also learn more about abdominal migraine and other types of migraine your family may experience by following the CEFALY blog. Our blog has expert-reviewed articles to help people with every type of migraine learn and thrive.
CEFALY is an FDA-cleared migraine device you can buy and use without a prescription. CEFALY is specifically indicated for the acute treatment of migraine with or without aura and the preventative treatment of migraine in patients 18 and older. While CEFALY is clinically proven to relieve migraine symptoms and reduce attack frequency, Its effectiveness for treating abdominal migraine has not been studied.
If you have abdominal migraine and want to use CEFALY, talk to your healthcare provider. Our 90-day guarantee means you can try CEFALY risk-free! If it doesn’t work for you, you may return it within 90 days of purchase.
Try CEFALY with a 90-day money-back satisfaction guarantee.















