Despite migraine affecting over a billion people worldwide and being the world’s third most common disease, insurance coverage for treatment is limited. If you experience migraine, you deserve effective preventive and acute treatments to help you reclaim your life. Insurance for migraine patients can be tricky territory, but this guide will help you navigate it. Be sure to also download the quick guide to insurance reimbursement for CEFALY.
How does insurance for migraine work?
Depending on your policy, insurance for people with migraine can involve some extra obstacles and considerations. These include step therapy, prior authorization and out-of-pocket expenses.
Step therapy
Many insurers have a step therapy or “fail first” policy. They require you to try one or more of their preferred treatments and show they don’t work before offering coverage for the treatment you want.
Each insurer chooses which treatments to designate for step therapy, and some are less stringent than others. Treatments that most often have fail-first requirements are:
- Injectable or oral calcitonin gene-related peptide (CGRP) inhibitors
- Botox injections
- Brand-name triptans
Prior authorization
Prior authorization means your insurer will only cover a treatment if you contact them for approval before getting it. This often applies to treatments or dosages different from what they usually cover, even if your doctor prescribes them. The preapproval process can be time-consuming, so submit your request promptly and follow up with your doctor and insurer.
Out-of-pocket expenses
Check your insurance policy to understand your financial obligations. Aside from your premiums, you may need to pay a deductible and co-payment to cover migraine treatment:
- Deductibles: These are the out-of-pocket amounts you need to pay toward a treatment before you can claim coverage for the rest.
- Co-payments: These are fees you must pay out-of-pocket for medical treatments while insurance covers the rest. Many insurers set high co-pays for migraine treatments, but some manufacturers offer payment plans or discount cards to help you afford your preferred treatment.
Try CEFALY for Migraine Relief
What migraine treatments are covered by insurance?
Each insurer makes its own decisions about what treatments to cover, but many have similar policies. Here’s how insurers tend to treat some common migraine treatments:
- Triptans: Generic triptans are often a preferred migraine treatment that insurers cover. Brand-name triptans are often subject to step therapy, meaning you may have to try a generic version first.
- Anti-CGRP monoclonal antibodies: Many insurers cover these, but with high co-pays and only after preapproval and/or step therapy.
- Botox: Many insurers will cover Botox for migraine, but it usually requires step therapy and prior authorization. Some insurers are becoming more open to covering Botox because of its proven effectiveness in treating chronic migraine.
- CEFALY: Insurance reimbursement for CEFALY varies by insurer and plan. The best way to find out if your insurance provider covers CEFALY is to contact your insurer directly and ask: “Does my plan cover durable medical equipment (DME) under HCPCS Code K1016?” If your insurer says yes, then ask: “What documents do I need to submit a claim?”
- Migraine glasses: Most insurers won’t cover migraine glasses. If you want to try them, you may need to use an FSA/HSA or pay out of pocket.
When will insurance not cover migraine treatment?
Insurers may refuse to cover migraine treatments for several reasons, including:
- Step therapy: If your chosen treatment is subject to a fail-first requirement, your insurer may deny your claim until you try their preferred treatment and show it doesn’t work.
- Off-label use: Several effective migraine treatments are only currently approved to treat other conditions. In these cases, insurers may regard them as experimental and refuse to cover them.
- Formulary changes: Many insurers adjust their list of covered treatments — called their formulary — annually. This could exclude your preferred treatment, even if they were covering it before.
- Layered therapies: Many people with migraine respond best to a combination of preventive and acute treatments. For example, research suggests a possible benefit of using Botox alongside anti-CGRP monoclonal antibodies to treat migraine. Layered therapies can treat some migraine cases better together than either can alone, but some insurers are only willing to cover one treatment at a time.
What if insurance denies my claim?
If your insurer denies your prior authorization or claim, you may still be able to get coverage by taking some extra steps. Here are your options:
- Contact your insurer: Try getting through to the pharmacy benefit manager — the person in charge of overseeing your plan benefits. Mention the treatment you want and why you want it. Ask about their criteria for considering treatment medically necessary. Be persistent, and record information about each conversation in case you need it to follow up or use as evidence later. Try to get copies of all communication in writing or an email.
- Submit an appeal: If your insurer denies a claim, they should notify you of the reason and let you appeal. Take note of the deadline and any other requirements for your appeal to be valid. If they deny the appeal, explore your options for following up with someone higher up in the company. You can also appeal to a third-party organization.
- Involve your doctor’s office: Your doctor can write a letter explaining why your preferred treatment is medically necessary. They could also assist you with your appeal and share medical data and studies that back the treatment. If you keep a migraine journal with your history, symptoms and responses to treatments, this can help your doctor make your case.
- Consider alternatives: Your efforts to get coverage for your preferred treatment may take a while. In the meantime, do what you can to prevent and relieve migraine. Work with your doctor to create an effective interim migraine management plan. Check if generic alternatives to brand-name drugs could get coverage. If you want a treatment before your insurer agrees to cover it, check if the manufacturer offers payment plans or discounts.
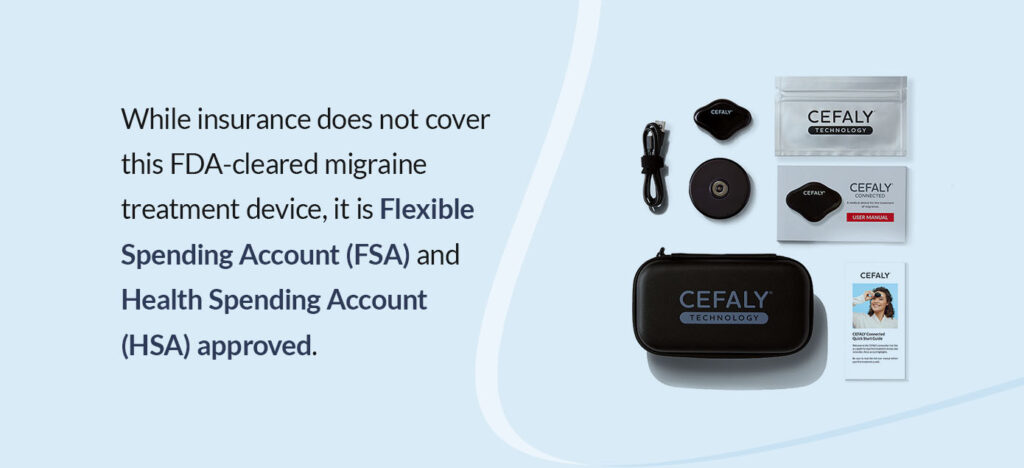
Order your CEFALY migraine treatment device online
CEFALY is an FSA/HSA-approved, FDA-cleared migraine treatment device that’s available without a prescription — buy it online anytime! Its preventive and acute treatment modes have clinical research backing their effectiveness. Plus, CEFALY is a drug-free treatment that’s safe to use alone or with medications.
Wondering if your insurance plan covers CEFALY? Here’s how to find out.
Even if you don’t have insurance coverage, CEFALY is a cost-effective migraine management option because:
- The only ongoing expenses are the low-cost reusable electrodes.
- You can use it without a prescription.
- We offer free shipping on device orders.
- Every device comes with a 90-day money-back guarantee if you aren’t satisfied with your results.
- You can apply for a monthly payment plan through Affirm and PayPal Credit.
Order CEFALY today to take control of your migraine treatment.